with hereditary AT deficiency have at least one clot by age 5010
with hereditary AT deficiency have recurrent blood clots10
- hATd affects 1 in every 500 to 5000 individuals9
- This range suggests that approximately 65,000 to 650,000 people in the United States are affected16
- Approximately 50% of individuals with hereditary AT deficiency will develop at least one clot in their lifetime (usually after adolescence).17
- 85% of patients with hATd will have at least 1 thrombotic episode by age 507
- ~70% of all patients with hATd will have a thrombotic event before the age of 357
- Up to 70% of pregnant women with hATd may experience thromboembolic complications18
- About 6 in 10 patients with hereditary AT deficiency have recurrent blood clots10
- Inherited blood-clotting disorders are diagnosed with a test called a thrombophilia panel. This test can help to diagnose hereditary antithrombin deficiency or another inherited blood-clotting disorder, like factor V Leiden, or protein C or protein S deficiency
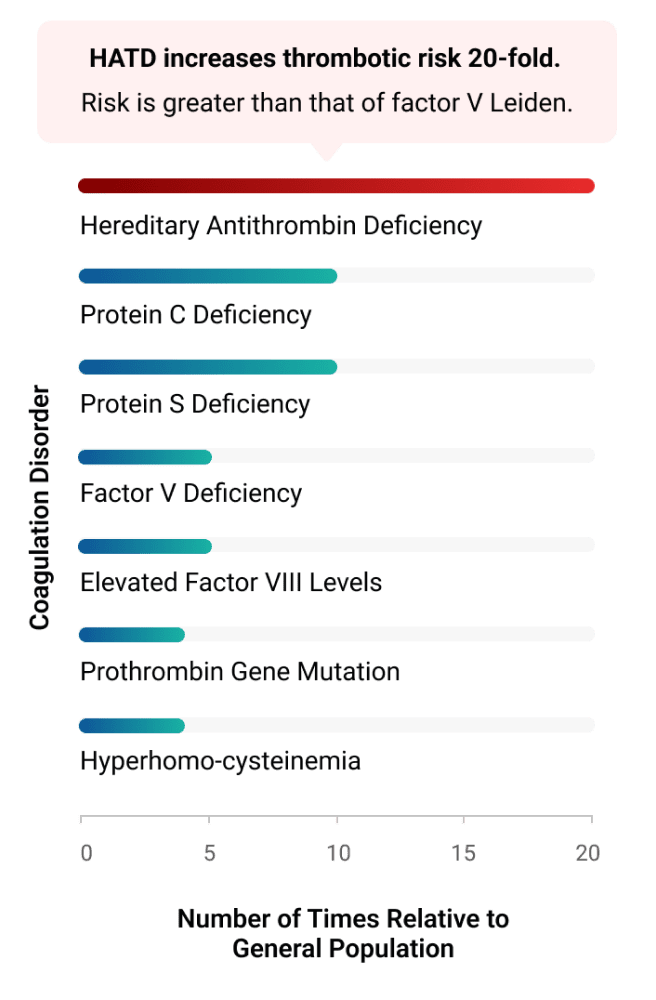
hATd has one of the highest thrombotic risks of all of the inherited thrombophilias19
hATd has 3 distinct features that set it apart from other thrombophilias
†Heparin and enoxaparin.
*Patients heterozygous for factor V Leiden have approximately a 5-fold greater risk of venous thrombosis, while homozygotes have approximately an 80-fold greater risk. Chart adapted from Franchini et al.
AT activity inhibits many clotting factors in the coagulation cascade in 3 key steps2-4
- Procoagulation factors bind to AT
- Once bound to AT, procoagulation factors are cleared
- The expansion of existing clots and formation of new clots are prevented
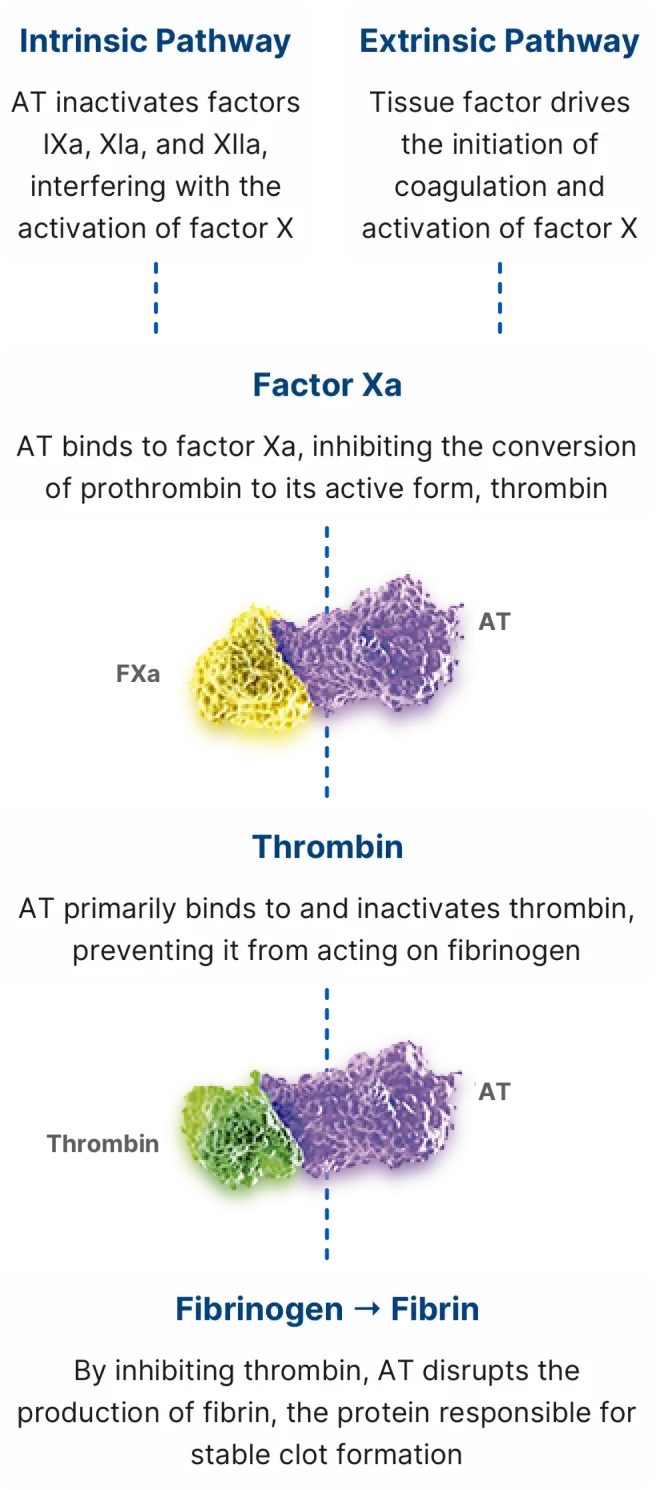
- Antithrombin is a thromboprotective protein that inhibits the coagulation enzymes in a slow, progressive manner when heparin is absent. These enzymes include factor Xa and thrombin, and to a lesser extent, factors IXa, XIa, XIIa, and VIIa25
- Antithrombin plays a key role in anticoagulation by preventing the activation of coagulation-promoting proteins except at the site of injury26
- Antithrombin participates in a feedback loop in which blood can clot rapidly when needed but does not clot all of the time26
THROMBATE III reduces VTE Risk
Dr. Bader talks about surgery in patients with hATd
Learn more about THROMBATE III
Have a question about THROMBATE III?
Get in touch with a representative today
Important Safety Information
THROMBATE III® (antithrombin III [human]) is indicated in patients with hereditary antithrombin deficiency for treatment and prevention of thromboembolism and for prevention of perioperative and peripartum thromboembolism.
Hypersensitivity reactions may occur. Should evidence of an acute hypersensitivity reaction be observed, promptly interrupt the infusion and begin appropriate treatment.
Because THROMBATE III is made from human blood, it may carry a risk of transmitting infectious agents, eg, viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent, and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. There is also the possibility that unknown infectious agents may be present in the product.
Perform coagulation tests to avoid excessive or insufficient anticoagulation and monitor for bleeding or thrombosis. Measure functional plasma AT levels with amidolytic or clotting assays; do not use immunoassays.
In clinical studies, the most common adverse reactions (≥ 5% of subjects) were dizziness, chest discomfort, nausea, dysgeusia, and pain (cramps).
The anticoagulant effect of heparin is enhanced by concurrent treatment with THROMBATE III in patients with hereditary AT deficiency. Thus, in order to avoid bleeding, the dosage of heparin (or low molecular weight heparin) may need to be reduced during treatment with THROMBATE III.
Please see full Prescribing Information for THROMBATE III.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit http://www.fda.gov/medwatch, or call 1-800-FDA-1088.
References
- THROMBATE III [Prescribing Information]. Research Triangle Park, NC: Grifols Therapeutics LLC
- Maclean PS, Tait RC. Hereditary and acquired antithrombin deficiency: epidemiology, pathogenesis, and treatment options. Drugs. 2007;67(10):1429-1440
- Li W, Johnson DJD, Esmon CT, Huntington JA. Structure of the antithrombin–thrombin–heparin ternary complex reveals the antithrombotic mechanism of heparin. Nat Struct Mol Biol. 2004;11(9):857-862
- James AH, Konkle BA, Bauer KA. Prevention and treatment of venous thromboembolism in pregnancy and patients with hereditary antithrombin deficiency. Int J Womens Health. 2013;5:233-241
- Wolberg AS. Thrombin generation and fibrin clot structure. Blood Rev. 2007;21(3):131-142
- Davi G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med. 2007;357(24): 2482-2494
- Kottke-Marchant K, Duncan A. Antithrombin deficiency: issues in laboratory diagnosis. Arch Pathol Lab Med. 2002;126(11):1326-1336
- Mitton BA, Steineck A. Antithrombin deficiency. eMedicine from WebMD. http://emedicine.medscape.com/article/198573-overview. Updated July 22, 2022. Accessed November 28, 2022
- Patnaik MM, Moll S. Inherited antithrombin deficiency: a review. Haemophilia. 2008;14(6):1229-1239
- Pabinger I, Schneider B. Thrombotic risk in hereditary antithrombin III protein C, or protein S deficiency. Arteroscler Thromb Vasc Biol. 1996;16(6):742-748
- Ranucci M. Antithrombin III: key factor in extracorporeal circulation. Minerva Anestesiol. 2002;68(5):454-457
- Foy P, Moll S. Thrombophilia: 2009 update. Curr Treat Options Cardiovasc Med. 2009;11(2):114-128
- AABB, American Red Cross, America’s Blood Centers, Armed Services Blood Program. Circular of information for the use of human blood and blood components. https://www.aabb.org/docs/default-source/default-document-library/resources/circular-of-information-watermark.pdf?sfvrsn=7f5d28ab_5 December 2021. Accessed November 28, 2022
- Tengborn L et al. Scand J Clin Lab Invest. 1981;41(5):469-477
- Wells PS, Blajchman MA, Henderson P, et al. Am J Hematol. 1994;45:321-324
- US Census Bureau, Population Division. US and World Population Clock. http://www.census.gov/ popclock/. Accessed November 28, 2022
- Khawar H, Kelley W,Guzman N. Fresh frozen plasma. In: StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK513347/. Updated September 19, 2022. Accessed November 28, 2022
- Hellgren M, Tengborn T, Abildgaard U. Pregnancy in women with congenital antithrombin III deficiency: experience of treatment with heparin and antithrombin. Gynecol Obstet Invest. 1982;14:127-141
- Franchini M, Veneri D, Salvagno GL, Manzato F, Lippi G. Inherited thrombophilia. Crit Rev Clin Lab Sci. 2006;43(3):249-290
- Rodgers GM. Role of antithrombin concentrate in hereditary antithrombin deficiency: an update. Thromb Haemost. 2009;101(5):806-812
- Di Minno MND, Dentali F, Lupoli R, Ageno W. Mild antithrombin deficiency and risk of recurrent venous thromboembolism. Circulation. 2014;129(4):497-503
- Bucciarelli P, Passamonti SM, Biguzzi E, et al. Low borderline plasma levels of antithrombin, protein C and protein S are risk factors for venous thromboembolism. J Thromb Haemost. 2012;10(9):1783-1791
- Centers for Disease Control and Prevention. Venous thromboembolism in adult hospitalizations – United States, 2007-2009. MMWR Morb Mortal Wkly Rep. 2012;61(22):401-404
- Finley A, Greenberg C. Review article: heparin sensitivity and resistance: management during cardiopulmonary bypass. Anesth Analg. 2013;116(6):1210-1222
- Kovács B, Bereczky Z, Oláh Z, et al. The superiority of anti-FXa assay over anti-FIIa assay in detecting heparin-binding site antithrombin deficiency. Am J Clin Pathol. 2013;140(5):675-679
- Olson E, Whitney M, Friedman B et al. In vivo fluorescence imaging of atherosclerotic plaques with activatable cell-penetrating peptides targeting thrombin activity, Integrative Biology, 2012;4(6):595–605
- Lloyd-Jones D, Adams RJ, Brown TM, et al; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2010;121:e46-e215